Meningitis has a devastating impact on health causing many deaths and often leaving survivors with serious long-lasting effects. Even with progress in medicine, it continues to pose a big threat to public health around the world. Outbreaks happen in many places in parts of Africa south of the Sahara.
Different things can cause meningitis such as bacteria, viruses, fungi, and parasites. Bacterial meningitis is worrying. About one out of every six people who get bacterial meningitis will die, and one in five will face severe problems afterward. To protect against this disease for a long time, vaccines that are safe and don’t cost too much work best.
Overview
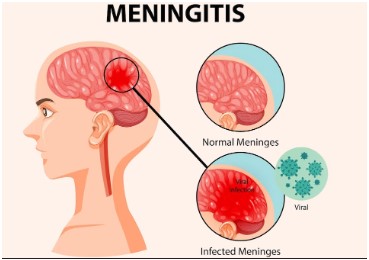
Meningitis causes swelling in the tissues that cover the brain and spinal cord due to an infection. It can kill you and needs quick medical help. Different germs like bacteria, viruses, fungi, and parasites can lead to meningitis.
Most infections spread from person to person, but a few cases happen because of injuries, cancers, or drugs. Bacterial meningitis, the most dangerous kind, can kill within a day and affects people of all ages. Even though we have good treatments and shots against some of the main bacteria that cause it, meningitis still poses a big threat worldwide.
There are four primary causes of acute bacterial meningitis:
- Neisseria meningitidis (meningococcus)
- Streptococcus pneumoniae (pneumococcus)
- Haemophilus influenzae
- Streptococcus agalactiae (group B streptococcus)
Meningitis worldwide has over 50 % of its cases caused by these specific types of bacteria while they may also trigger conditions such as sepsis or even pneumonia. More significant causes consist of Mycobacterium tuberculosis, Salmonella, Listeria, group A Streptococcus, Staphylococcus, enteroviruses, mumps virus, Cryptococcus fungi or parasites belonging to Amoeba.
Who is at Risk of Menengitis?
Meningitis can strike people of all ages, but kids face the highest danger. Babies have a special weakness to Group B streptococcus. Young kids tend to catch infections from meningococcus, pneumococcus, and Haemophilus influenzae and more .
Teenagers and young adults have a greater risk of getting meningococcal disease and the elders are likely to get pneumococcal disease. People who live close together have a higher chance of getting sick. This includes those in big crowds, refugee camps packed houses, or certain work places like college dorms and army barracks. Other things that make you more likely to get sick include weak immune systems (like with HIV) suppressed immune systems, and smoking or being around smoke.
Transmission of Menengitis
The way an organism spreads changes based on its type. Most bacteria that cause meningitis, like meningococcus, pneumococcus, and Haemophilus influenzae, live in people’s noses and throats. These bacteria spread through tiny drops from the respiratory system or secretions from the throat. Group B streptococcus often lives in the human gut or vagina and can pass from mother to baby during childbirth. While carrying these organisms doesn’t hurt and helps build up immunity. However sometimes the bacteria get into the body leading to meningitis and sepsis.
Signs and Symptoms
The clinical features of meningitis vary depending on the cause and progression of the disease. Common symptoms include neck stiffness, fever, confusion or altered mental status, headaches, nausea, and vomiting. Less frequent symptoms are seizures, coma, and neurological deficits such as hearing or vision loss, cognitive impairment, or limb weakness.
Bacterial meningitis pathogens can also cause symptoms due to bloodstream infections (septicaemia), quickly leading to sepsis, which includes cold hands and feet, joint and muscle pains, faster than usual breathing, diarrhea, and a dark purple or red rash.
In infants, symptoms can include being less active and difficult to wake, irritability, poor feeding, a stiff or floppy body, and swelling in the soft spot of the head (fontanelle).
Complications and Sequelae
One in five people surviving bacterial meningitis may experience long-lasting after-effects, such as hearing loss, seizures, limb weakness, vision and speech difficulties, memory and communication challenges, scarring, and limb amputations following sepsis. The impact on individuals, families, and communities can be significant, both financially and emotionally.
Prevention of Menengitis
Immunization provides excellent immunity over standard forms of bacterial meningitis. There are licensed immunizations for meningococci, pneumococci and Haemophilus influenzae type b (Hib).
This form of vaccination has been directed towards the most dangerous strains of bacteria. In the meningitis belt region within Africa, mass preventive campaigns and normal immunization programmes have drastically lowered cases meningococcal A epidemics.
Antibiotics for Prevention (Chemoprophylaxis)
When given timely to those who have had close contact, antibiotics can avert the transmission of meningococcal illness. The preferred antibiotic is ciprofloxacin, and ceftriaxone may be used alternatively. It is advisable to identify mothers at risk of giving birth to infants vulnerable to Group B streptococcal infection, although intravenous penicillin can safeguard newborns against infection during labor.
Diagnosis
Diagnosing meningitis involves a clinical examination followed by a lumbar puncture to analyze the cerebrospinal fluid. Bacteria can sometimes be seen in microscopic examinations of the spinal fluid. Diagnosis is confirmed by growing bacteria from specimens of cerebrospinal fluid or blood, using rapid diagnostic tests or polymerase chain reaction (PCR).
Identifying the serogroups and susceptibility to antibiotics is crucial for defining control measures. Molecular typing and whole-genome sequencing help identify strain differences and inform public health responses.
Treatment of Menengitis
Meningitis has a significant impact on health and needs quick medical care. Bacterial meningitis requires antibiotics right away. Viral and bacterial meningitis can look alike, but they differ in how bad they are and how doctors treat them. Anyone showing signs of meningitis should go to a hospital or health center at once. This helps doctors figure out what’s wrong and give the right treatment and care.
Long-Term Impact and Support
Meningitis aftereffects can change the lives of people, their families, and their communities. Those who’ve beaten meningitis often need long-term medical care. The lasting mental and social effects of meningitis-caused disabilities can limit schooling social life, and job chances.
Getting help and support for these issues is often hard in poorer countries. Families should ask local and national Disabled People’s Groups (DPGs) and other disability-focused groups for help with legal rights, job opportunities, and social activities.
Surveillance and WHO Response
Keeping an eye on meningitis plays a key role in managing the disease, from spotting cases to backing them up in the lab. The goals? To spot and confirm outbreaks, track how often it happens, figure out how big the problem is, and see how well control plans work when it comes to vaccines.
The WHO’s big plan, “Beating Meningitis by 2030,” wants to wipe out bacterial meningitis outbreaks, cut down cases that vaccines can prevent by half, and deaths by 70%. It also aims to make life better for people dealing with meningitis. This far-reaching plan involves teaming up with lots of partners and countries to tackle the tough spots and fill in the gaps in caring for and helping folks with meningitis and other brain-related issues around the world.
Meningitis continues to pose a major threat to global health killing many and leaving survivors with serious lasting effects. Vaccines offer the best defense against bacterial meningitis. People with this condition need quick medical care and the right treatment. To beat meningitis around the world, we must keep watching for outbreaks, take steps to prevent them, and help those who’ve had the disease.